In the first part of our story (click here) we saw how there are three different types of carbohydrate and that each has a very different effect on our blood sugar levels once eaten.
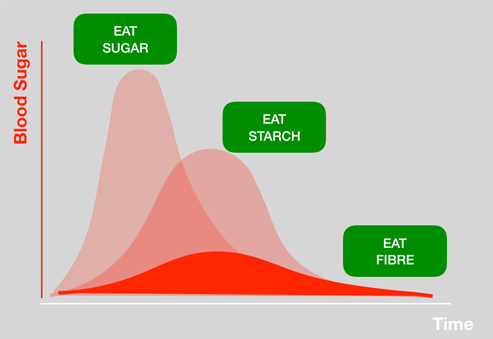
Our body biochemistry does not like our blood sugar levels to be raised too high or for too long and so we have evolved a mechanism to deal with it. This is where insulin comes in. Insulin is a hormone produced by the pancreas and released in response to raised blood sugar levels that brings our blood sugar levels down once they have been raised.
The peak amount of insulin produced (in someone who has a fully functioning insulin system) is in proportion to the amount of blood sugar rise.
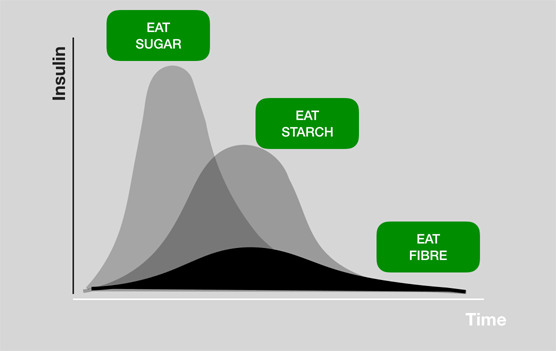
This insulin response to consumed sugars and starches is quite normal and part of our evolved response to sugars and starches in our diet. However, problems arise when this insulin mechanism becomes over-used.
Over most of the evolution of homo sapiens we have only had access to sugars and starches in small amounts and at specific times of year – autumn berries and the winter root vegetables being the main sources.
Of course we now have access to those forms of sugar and starch all year round and also lots of refined starches and sugars in breakfast cereals, cakes, biscuits, chocolates, fruit juices, sodas. Our insulin mechanism is being called upon all the time to mop-up the surges in blood sugar caused by each of these foods.
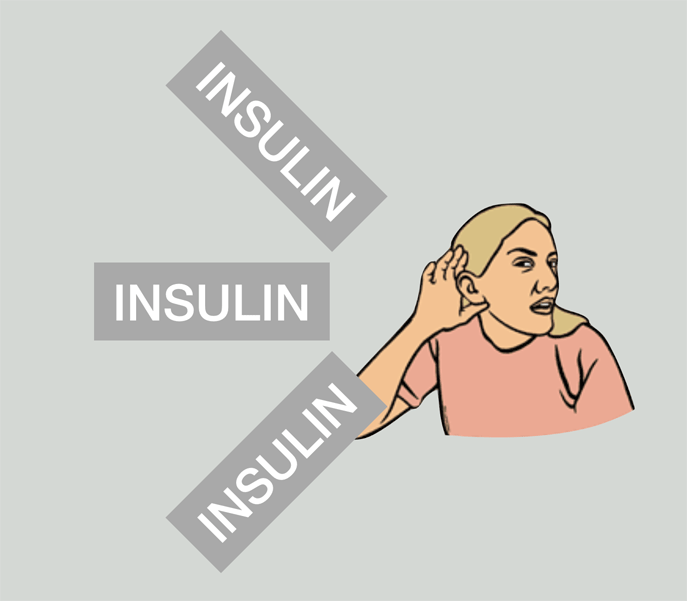
Changes then occur in our insulin response to continually raised blood sugar levels. The cells in the body that should respond to the insulin message to bring down blood sugar levels become a little bit deaf to the message of insulin. It is a bit like the naughty child who is persistently reprimanded by a parent but that child then starts to become immune to the reprimands because they are constant. And just as the parent has to shout a little louder to get their message across, so our body has to ‘shout’ its insulin message a little harder to get its message across.
This is the start of Insulin Resistance (I.R.).
If I.R. is allowed to develop and progress unchecked, eventually the pancreas can no longer produce enough insulin to get its message across. This is the onset of Type II Diabetes. Where this condition develops the body can no longer control blood sugar level surges and harmful levels of glucose in the blood go un-checked. This can lead to a host of serious medical consequences many of which over a long period of time are life-altering and indeed life-threatening.
But our problems with sustained levels of insulin in the body are not solely a result of Type II Diabetes. Insulin for example is a key hormone signal telling the adipose (fat-storing) cells in the skin to take up excess glucose and fatty acids and add them to the fat reserves. High and continuously high levels of insulin therefore encourage you to get fatter!
Sustained high levels of insulin also change your energy metabolism. Our bodies can use both glucose and fats to derive energy – the fats that are used for energy can be in the form of ketone bodies which is why this way of energy burning is often termed ‘ketosis’. If there are continuous high levels of insulin in the blood, this reduces the level of ketone production and consequently fat metabolism and at the same time promotes sugar/glucose metabolism.
This can be problematical:
- Ketone bodies are essential for brain maintenance and development; limiting their supply as a consequence of high levels of insulin will therefore have neurological consequences.
- Our bodies can only store around 2000 calories in the form of sugars; we can however store 20-30,000 calories as fat. Relying on sugars for energy requires constant replenishment whereas a low insulin fat burning metabolism allows us to continue for much longer without eating.
- Sugar metabolism (driven by sustained high levels of insulin) produces chemicals called Reactive Oxidative Species (R.o.S) and these are, when allowed to accumulate, inflammatory. A low insulin, fat burning regime keeps the levels of R.o.S. low and thereby reduces inflammation. Sustained chronic inflammation is correlated with the development of many chronic health conditions.
- The sustained level of blood sugar leads to glucose molecules attaching to protein molecules creating AGE (Advanced Glycolation End products). These ‘foreign’ molecules can trigger the body’s auto-immune response and over a long period of time this leads to an impaired response leading to the development of other auto-immune conditions.
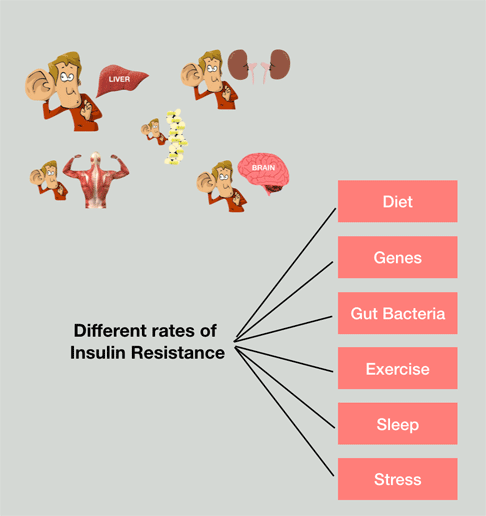
The development of Insulin Resistance is not just down to the amount of starch and sugar that you eat. Whilst that is a very significant factor there are many other factors each of which contribute and probably contribute to a different extent in each one of us. The diversity of gut bacteria, the quality of sleep, the amount of stress in your life are all factors that contribute.
So, if consuming large amounts of starch and sugar on a regular basis is a key contributing factor correlated to a whole host of chronic illness, how can we manage our diet to mitigate this? Read more in the next article.